יום הזיכרון לשואה ולגבורה
בית הטכניון מוזמן לעצרת זיכרון לשואה ולגבורה שתתקיים ביום ה' בשעה 09:45 באולם צ'רצ'יל ובמהלכה תתקיים הרצאתו של יוסי פלד (אלוף במיל'), שורד שואה שיספר את סיפור חייו.

בית הטכניון מוזמן לעצרת זיכרון לשואה ולגבורה שתתקיים ביום ה' בשעה 09:45 באולם צ'רצ'יל ובמהלכה תתקיים הרצאתו של יוסי פלד (אלוף במיל'), שורד שואה שיספר את סיפור חייו.

המוקדים עוסקים במגוון תחומים ובהם אנרגיה, תזונה, מערכות מים, איכות מים ופרוטאומיקה.

פרופ' חוסאם חאיק, דיקן לימודי הסמכה וחבר סגל בפקולטה להנדסה כימית ע"ש וולפסון בטכניון, זכה בפרס הבין-לאומי היוקרתי המוענק על ידי אגודת מחקר החומרים


טקס לציון יום הזיכרון לשואה ולגבורה
24.04.2025 חמישי, בשעה 09:45
הוספה ליומן

טקס יום הזיכרון לחללי מערכות ישראל ופעולות איבה וטרור
29.04.2025 שלישי, בשעה 11:00
הוספה ליומן
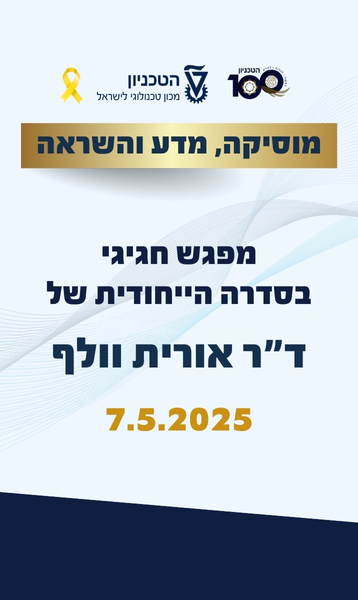
מוסיקה, מדע והשראה - הסוד מאחורי השראה: מדענים ואמנים בשיחה פתוחה
07.05.2025 רביעי, בשעה 15:00
הוספה ליומן

יום יזמות, קריירה וחברה ויריד תעסוקה
13.05.2025 שלישי, בשעה 08:00
הוספה ליומן

פסטיבל הסטודנט המשותף בטכניון
21.05.2025 רביעי, בשעה 20:00
הוספה ליומן
100000
בוגרים
18
פקולטות
15000
סטודנטים
60
מרכזי מחקר
ברחבי הקמפוס