יום פתוח בטכניון
בואו להכיר מקרוב את הטכניון ביום הפתוח ב-5/3 בקמפוס הטכניון בחיפה

הרצאתו של ד"ר יותם בר-און מהפקולטה לרפואה ע"ש רות וברוך רפפורט : מדוע הנגיפים תמיד מנצחים?

מדד CSRankings מדרג את הטכניון במקום הראשון באירופה בתחום ה-AI על פי נתוני 2025-2005

האסטרופיזיקאי שפרד דואלמן, שהוביל את הצילום הראשון של חור שחור, אמר לסטודנטים בטכניון כי אחת המשימות הבאות היא צילום סרטון וידאו של חור שחור

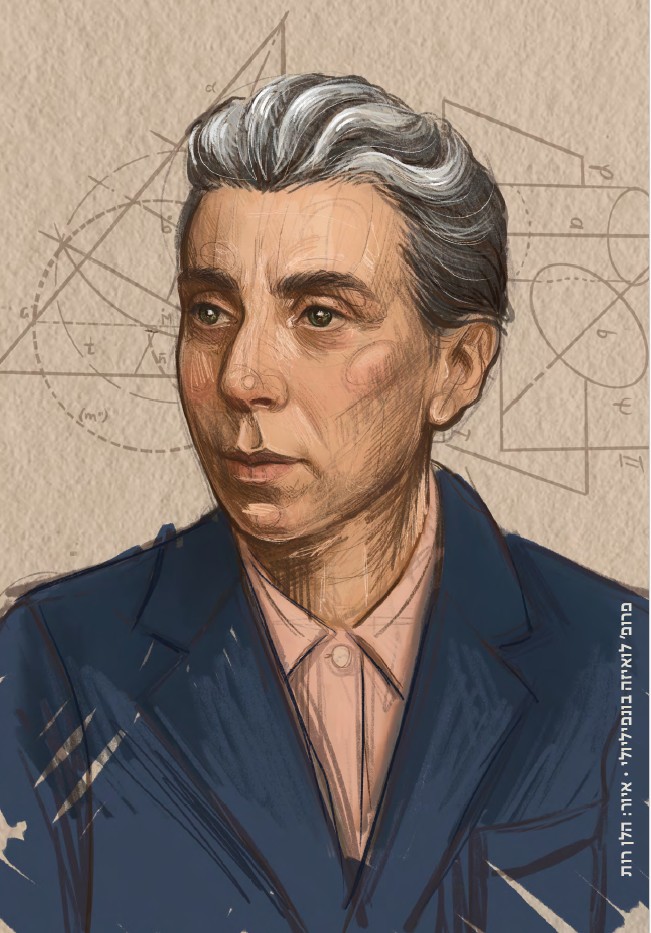
כנס LadyTech12
23.02.2026 שני, בשעה 18:00
הוספה ליומן

כנס תכנון ובניה - חיפה והצפון 2026
24.02.2026 שלישי, בשעה 08:30
הוספה ליומן

הכנס הישראלי השני לפילוסופיה של בינה מלאכותית
04.03.2026 רביעי, בשעה 09:30
הוספה ליומן

יום פתוח בטכניון 5.3
05.03.2026 חמישי, בשעה 09:30
הוספה ליומן
תערוכת "מראות מקום"
30.11.2025 ראשון, בשעה 09:00
הוספה ליומן

תערוכת הצילום "טבע בקמפוס"
16.07.2025 רביעי, בשעה 09:00
הוספה ליומן
100000
בוגרים
18
פקולטות
15000
סטודנטים
60
מרכזי מחקר
ברחבי הקמפוס